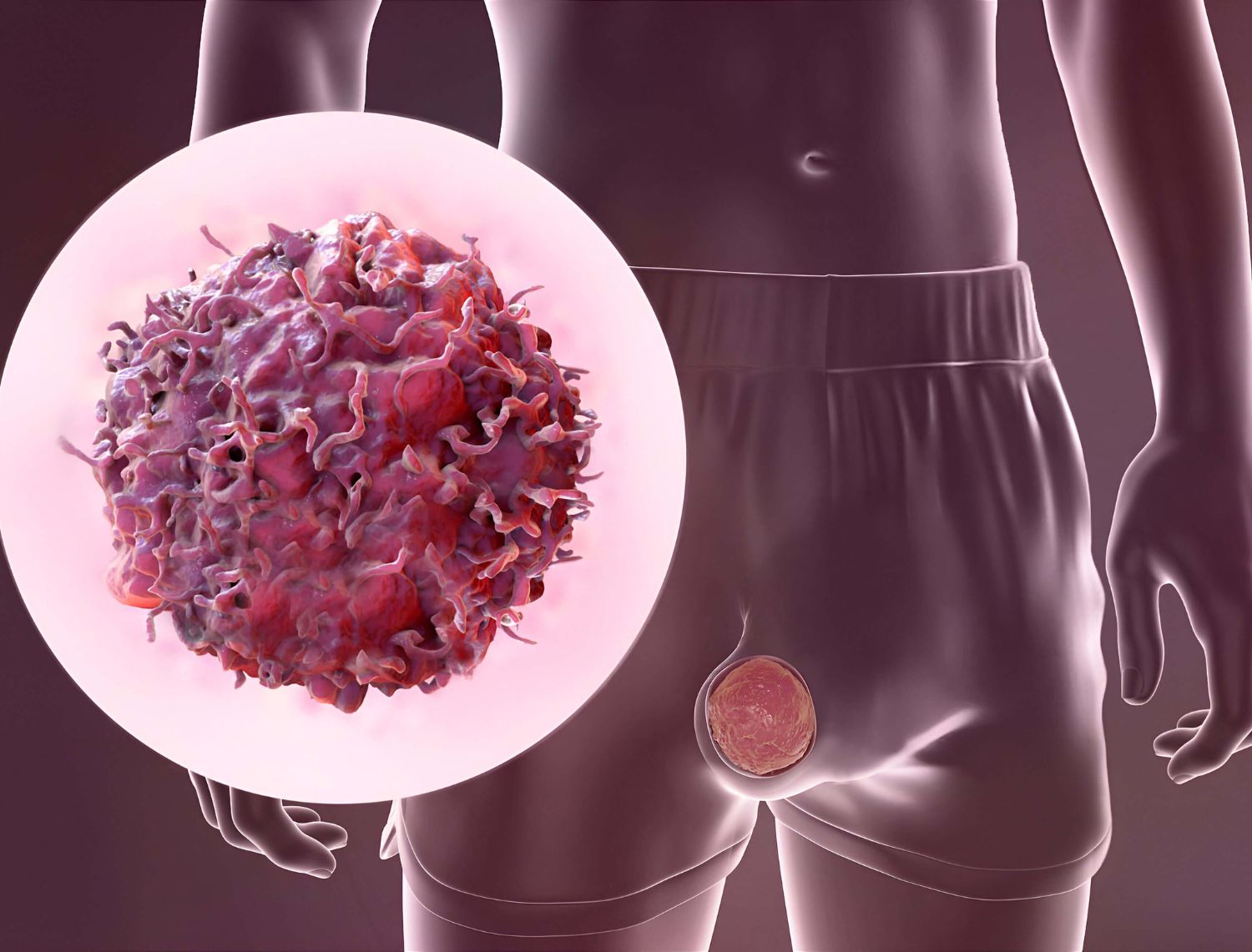
The initial step typically involves examining the testicles for any signs of swelling, lumps, or abnormalities in size and texture.
This imaging technique uses high-frequency sound waves to create detailed images of the testicles and scrotum. It helps to determine the nature of any lumps, whether they are solid (likely cancerous) or filled with fluid (likely non-cancerous).
Certain proteins, known as tumour markers, can be elevated in the blood when testicular cancer is present. Common markers include alpha-fetoprotein (AFP), beta-human chorionic gonadotropin (β-hCG), and lactate dehydrogenase (LDH).
If cancer is confirmed, additional imaging tests like CT scans or MRIs might be used to check if the cancer has spread to other parts of the body.