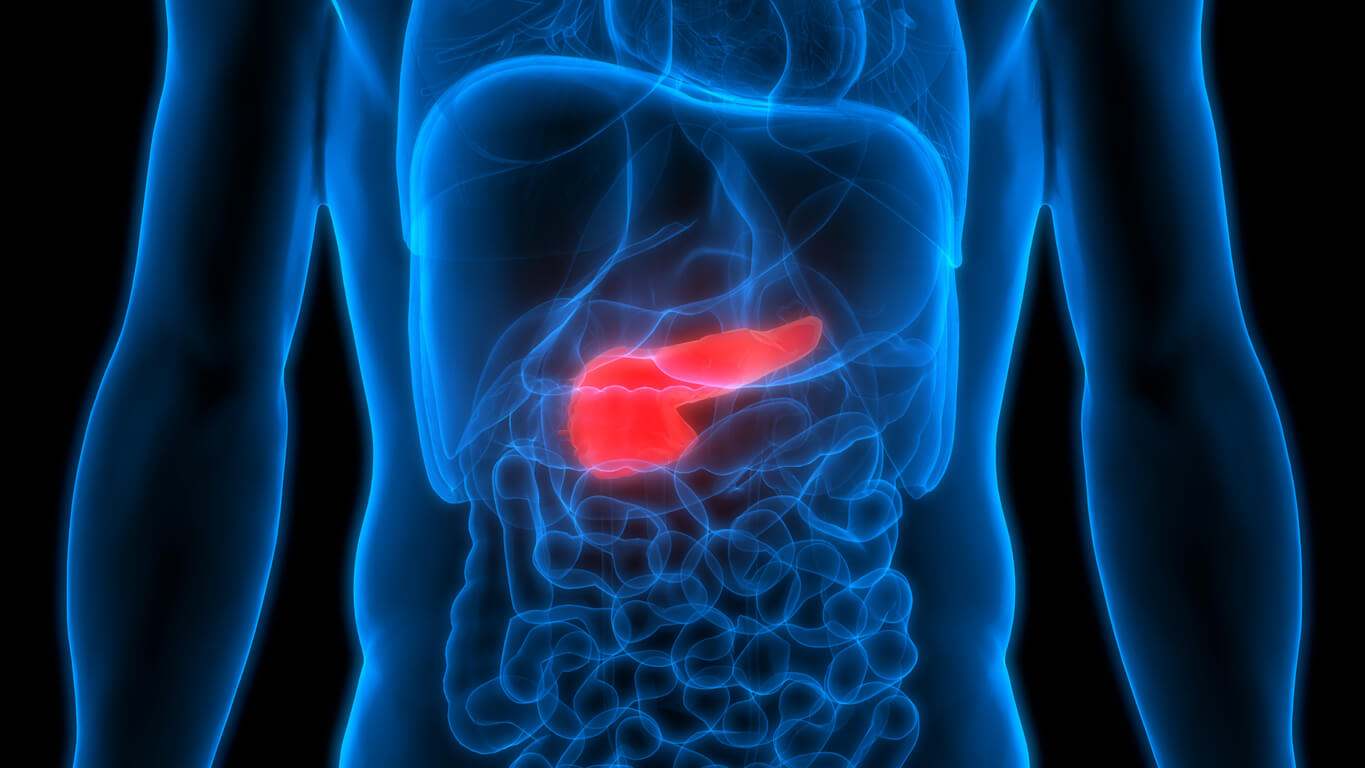
1. Incision: The surgery begins with the surgeon making an incision in the abdomen to access the pancreas.
2. Removal Of Tissues: The head of the pancreas, duodenum, gallbladder, and bile duct are removed. Parts of the stomach and nearby lymph nodes may also be excised.
3. Reconstruction and Suturing: After removing the necessary tissues, the surgeon reconstructs the digestive system by attaching the remaining pancreas, bile duct, and stomach to the small intestine, ensuring the continuation of digestive processes. Lastly, the surgeon sutures the incision made at the beginning of the surgery.